AI and its related tech have changed the way healthcare works across all departments and…

Personalized Patient Care: Why It Matters and How to Achieve It
Ever felt like a number in the healthcare system? The fact is that patients expect more, and healthcare organizations need to accept this as soon as possible.
Last year, 88% of patients said they want healthcare as tailored as their online shopping experience. Sounds like a high bar, until you realize it’s now the baseline.
Personalized healthcare is a massive shift that nets trust, better health outcomes, optimized resource planning, and a whole lot more, especially in digital and value-based models. Here’s what you need to know.
The Need for a Personalized Approach to Patient Care
The best way to differentiate the two is to think of traditional care as a template approach. Patients are treated as numbers that the staff needs to process as quickly as possible. Their individual markers and differences, behavior patterns, and environments are not considered at all. Hence, providers end up delivering generic care that often leads to avoidable mistakes.
Personalized care addresses the problem with great efficiency. It uses each patient’s medical history, lifestyle, and preferences to guide decisions, cutting out unnecessary tests, repeat visits, and hospital stays.
A recent review notes that such a personalized approach in healthcare can save the United States up to $200 billion a year. These are measurable gains that healthcare organizations can’t ignore.
Personalization matters in digital and value‑based models because both emphasize efficient, patient-centered outcomes, not volume of services. It makes each patient’s data work for them, reducing waste, minimizing harm, and increasing value.
Benefits of Personalized Patient Care
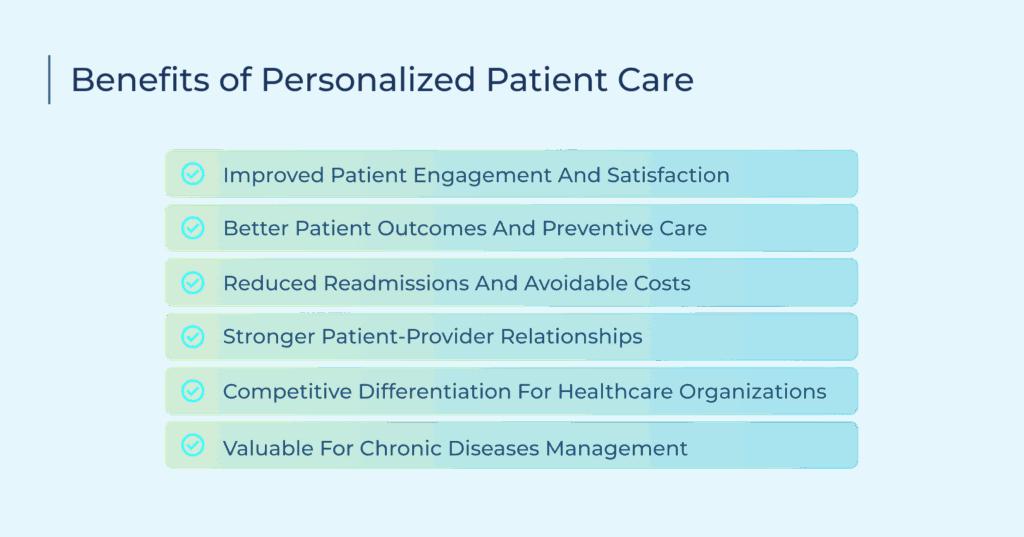
Personalized care isn’t just about high satisfaction scores. It leads to measurable improvements across multiple areas of care. Here are some of the most common improvements healthcare organizations see when they focus on personalization.
Improved Patient Engagement and Satisfaction
Healthcare providers can only form trusting relationships when patients receive care that acknowledges their unique situations. For instance, a new mother will appreciate relevant guides about infant care instead of generic wellness tips. This relevance creates stronger patient-provider connections.
The same approach also helps improve response rates. Even tailored care needs to follow preferred channels. Some patients prefer text messages. Others want phone calls. A multi-channel communication approach ensures no one is left behind. For providers, that becomes a surgical effort: precise, timely, and aligned with patient engagement.
Better Patient Outcomes and Preventive Care
Personalized care is highly efficient in catching early warning signs. Patients with a known family history of diabetes or heart disease can be specifically screened for blood sugar levels, cholesterol, and blood pressure, making it easier for providers to intervene before major issues develop.
These targeted solutions remove obstacles that normally prevent good health outcomes. Patients also leave happy, not only because they start recovering faster, but because their treatments match their lifestyles. Medication reminders, for example, work best when they arrive at times when patients have to take their pills.
Reduced Readmissions and Avoidable Costs
When health outcomes improve, readmissions take a dive. Personalized follow-up makes sure each patient goes home with a complete understanding of their health condition. Providers are also able to identify high-risk patients, such as post-surgical heart patients, giving them specific care instructions and check-in schedules.
This personalization ensures that patients adhere to their medical advice, improving their recovery and reducing the chance of them being readmitted for the same issue. Hence, saving costs for both sides.
Stronger Patient-Provider Relationships
Personalization is all about crystal clear and focused communication, but it goes a lot deeper than just remembering names and birthdays. Providers who remember patient preferences, needs, and previous conversations create stronger bonds.
Someone who comes in with a complaint of heart flutters, but has mentioned stress in the past, needs a physician who can connect the dots, not just throw generic responses. This is more effective than throwing down generic statements. Matching your message frequency and tone to each patient’s condition also keeps them engaged and more likely to stay.
Competitive Differentiation for Healthcare Organizations
Personalization attracts and retains patients, which automatically becomes a competitive edge in the community. Patients will always choose providers who give them time and attention over those who use standard protocols to rush through each patient to clear the waiting room before lunch. That difference becomes a clear advantage in word-of-mouth recommendations.
Additionally, healthcare organizations that improve their brand perception of personalized care attract patients who seek more than basic medical services. These patients often have higher engagement with preventive care and better insurance coverage, creating more sustainable patient populations.
Market positioning becomes clearer with personalized care offerings. Organizations can differentiate based on individualized service rather than competing solely on location or insurance acceptance. This differentiation supports premium pricing for enhanced service levels.
Valuable for Chronic Diseases Management
Tailored care plans address specific challenges each chronic disease patient faces. In the case of remote monitoring, blood pressure patients receive monitoring schedules that fit their daily routines. Glucose testing reminders arrive when patients typically eat meals. Medication alerts consider work schedules and sleep patterns.
Coaching and education match individual learning preferences and health literacy levels. Some patients prefer detailed written materials. Others learn better through videos or phone conversations. Educational content addresses specific patient concerns rather than general disease information.
Disease progression tracking improves with individualized baselines and goals. Providers set realistic targets based on patient capabilities and circumstances. Progress measurements account for individual factors affecting health outcomes.
How to Offer Personalized Patient Care as a Healthcare Provider
More and more patients are starting to expect treatment plans based on their preferences and needs. This puts healthcare providers under mounting pressure to deliver beyond their standard care protocols. However, implementing personalized care involves multiple components at different levels, all working together like a single cohesive machine.
Leverage the Patient Data Effectively
Start tailoring your approach with EHRs. They contain detailed information about every patient: medical history, allergies, medications, treatment responses, etc.
A patient with several medication allergies can have their prescriptions heavily filtered. Someone with a history of treatment non-compliance would be a prime case for more frequent check-ins and simplified medication schedules.
Segment and Prioritize Patients Based on Risk
Group patients based on their individual risk factors. The ones at the top, often with multiple chronic conditions, require intensive monitoring. Stable chronic cases also need regular check-ins, but less oversight in comparison. Each group needs tailored communication and care protocols.
Use of AI and Automation to Scale Personalization
AI makes personalization easier to implement and manage at scale. It can go through thousands of lines of patient data within seconds to find any concerning patterns. Hence, doctors get a smart pair of eyes to predict health risks.
Beyond care, automated communication systems send personalized messages based on patient profiles and care protocols. Appointment reminders arrive through preferred communication channels at optimal times. Medication adherence messages include specific drug names and dosing instructions.
Chatbots handle routine patient questions using individual health information to provide relevant responses. This automation allows care teams to focus on complex patient needs while maintaining consistent communication with entire patient populations.
Tailored Communications for Better Patient Engagement
Use the most appropriate communication channels based on the message being delivered. Most patients prefer text messages for appointment reminders and quick updates. Sending those via email would just be a poor notion of personalized care. Instead, use email for sharing educational materials.
Additionally, message timing also affects response rates and engagement. You can’t expect a working patient to manage their appointments during business hours.
Use of Remote Monitoring Technology
Wearable devices and connected health tools provide continuous patient data that informs care decisions. They also create opportunities for immediate intervention when patient data shows concerning trends. Blood pressure spikes trigger care team alerts and patient outreach. Irregular medication timing prompts adherence coaching. Providers use this information to make proactive care adjustments rather than waiting for scheduled appointments.
Personalized Education and Coaching for the Patients
Personalized care doesn’t stop at diagnosis. It shapes how information is delivered and support is offered. Education materials should align with how each patient processes information. It can be either video content, step-by-step guides, or in-depth reading.
Coaching adjusts to fit patient behavior and circumstances. Some need structure and regular follow-ups; others prefer autonomy with optional tools. The goal stays the same: remove friction, meet patients where they are, and make care easier to follow.
Foster a Culture of Personalized Care Throughout the Organization
Staff training and workflows both support personalized care. Team members learn to adapt based on patient needs, communication styles, and backgrounds. Systems and forms capture and share relevant details across departments. Leadership reinforces this through clear priorities, resource support, and performance tracking tied to patient experience.
Examples of Personalized Patient Care
Personalized care takes many forms, depending on patient needs, behaviors, and preferences. Below are several practical ways healthcare organizations are applying it today.
Virtual Health Assistants: We’ve already established how AI-driven automation makes patient communication far more effective. These smart assistants handle routine questions and provide post-visit instructions based on each patient’s situation.
Custom Medication Reminders: Speaking of aligning with each patient’s situation, providers are now sending reminders to patients to check their blood pressure or sugar levels at optimal times that align with their personal schedules.
Personalized Discharge Instructions: The days of handing a printout of generic discharge instructions are long gone. Patients now receive guidelines that are tailored to their health conditions and environments, including warning signs to watch for.
Proactive Health Monitoring: Healthcare now comes to you in far-flung, remote areas. Patients only need to track their vitals through wearable devices. They automatically alert healthcare teams when readings become concerning. The great thing about this is that the system considers individual baselines rather than generic thresholds.
Condition-Based Education Content: Providers are done with generic educational materials. Patients now receive tailored content that matches their diagnosis, learning style, and literacy level.
Addressing the Personalized Patient Care Challenges
Personalized care depends on data, which includes patient preferences, communication styles, wearable feeds, etc. It also includes managing all this across systems, channels, and teams that can break workflows.
Providers face inconsistent communication, technical bottlenecks, and outdated staff processes. TeleVox, as a market leader in tech-based healthcare solutions, tackles these issues by automating workflows and channeling communications via its SMART Agent and Digital Care Programs.
That means reminders, follow-ups, and education flow consistently through text, voice, or email, without adding burden to staff.
Security, integration, and AI trust remain top concerns. TeleVox ensures AI only shares provider‑approved content and links directly with EHRs, preventing misinformation or misrouting.
Implementation comes with tools and support. Leadership can track quality metrics, monitor patient satisfaction, and reward staff. With TeleVox, personalization stays precise, coordinated, and compliant, yet simple enough to run smoothly.
Future Trends of Personalized Healthcare
Personalized care is becoming the new baseline. There’s a surging demand for providers to know exactly their patients’ preferences, anticipate needs, and respond quickly.
AI tools, predictive analytics, and conversational agents are moving this expectation into daily operations. Virtual-first care is also expanding, giving patients direct access to tailored support without stepping into a clinic. These trends aren’t distant. They’re already shaping how care is delivered, measured, and experienced.
Healthcare organizations that delay adaptation risk falling behind. Those still relying on generic outreach and static care plans will lose patient trust and revenue. It’s now a race to stay relevant in a system where personalization will soon define standard care.