A patient engagement platform is a digital hub that makes it easier for patients to…

EHR Integration With Patient Relationship Management (PRM) for Better Outcomes
While Electronic Health Records (EHRs) are essential for organizing clinical data, they often fall short in supporting personalized, ongoing patient engagement. Many systems struggle with one-size-fits-all communication, limited outreach capabilities, and barriers for patients with low digital access.
That’s where Patient Relationship Management (PRM) platforms step in to close these gaps, enabling smarter, more personalized interactions that improve patient relationships, satisfaction, and ultimately lead to better health outcomes.
What’s Patient Relationship Management (PRM)?
PRM is a strategy intended to foster long-term, personalized relationships with patients through sustained, meaningful, and bi-directional communications. Like customer relationship management (CRM), PRM puts the consumer/patient at the center, rather than a one-way street that benefits only the health institution.
However, PRM transcends traditional patient engagement by replacing episodic touchpoints with continuous, data-driven interactions that span the entire healthcare journey. Communication is a critical component here. Unlike episodic patient engagement, PRM focuses on sustained connection to enhance overall experiences and outcomes. This puts the health provider on a track to deliver financial success through patient success.
Limitations of the EHR
EHRs are comprehensive systems for managing the vast amount of medical data generated throughout a patient’s care, including medical histories, treatment records, and diagnoses. While they efficiently organize clinical information, their capabilities stop at basic data management.
Most EHRs handle simple communications: appointment reminders, lab result notifications, and billing alerts. These features meet minimal requirements but fail to address complex patient needs. Here’s where most EHRs fall short:
- Personalized Communication: While some EHRs, like Epic’s CRM, now include outreach tools, they tend to rely on standardized templates and offer limited personalization.
- Tracking Preferences: Some EHRs have summary pages for patient information, but comprehensive tracking of communication across multiple touchpoints remains severely limited.
- Patient Insights: Most EHRs feature feedback tools, but often lack robust, real-time engagement analytics.
- Feedback Collection: EHRs may gather simple patient surveys, but their flexibility and depth in analyzing experiences vary significantly.
- Behavioral Data Integration: Most modern EHRs still struggle to link clinical data with behavioral patterns that go a long way in influencing health outcomes.
Healthcare organizations relying solely on EHRs for patient engagement tend to fall short when building trust and improving adherence to treatment plans for better health outcomes.
How EHR Integration With PRM Improves Patient-Provider Relationship
PRMs and EHRs work together to prioritize positive patient experiences that go beyond basic record-keeping. An EHRs’ main purpose is to store and manage clinical data. PRMs, on the other hand, provide solutions to build meaningful connections with both current and new patients through personalized interactions at every touchpoint in their healthcare journey.
On their own, EHRs often end up creating cookie-cutter interactions. Think of it as a one-size-fits-all approach that fails to address the diverse needs and preferences of individual patients.
Hence, when combined with PRMs, healthcare organizations get a platform that creates targeted communication to address specific patient needs. Here are a few examples to show how that works:
- Appointment reminders that consider patient communication preferences stored in the EHR.
- Post-visit follow-ups with customized care instructions and satisfaction surveys.
- Preventive care alerts that identify and notify patients with gaps in recommended screenings.
- Automatic rescheduling options are sent after missed appointments.
- Condition-specific check-ins for patients with chronic diagnoses.
- Communications in the patient’s preferred language as documented in their record.
- Feedback requests tailored to specific visit types or procedures.
- Personalized outreach to reconnect with inactive patients.
Best Practices for Integrating PRM Tools With the EHR
A PRM-EHR integration still needs optimized workflows to perform as expected. EHR is a natural technology pairing for PRM tools, but thoughtful implementation is essential. Below are some key considerations for providers in that regard.
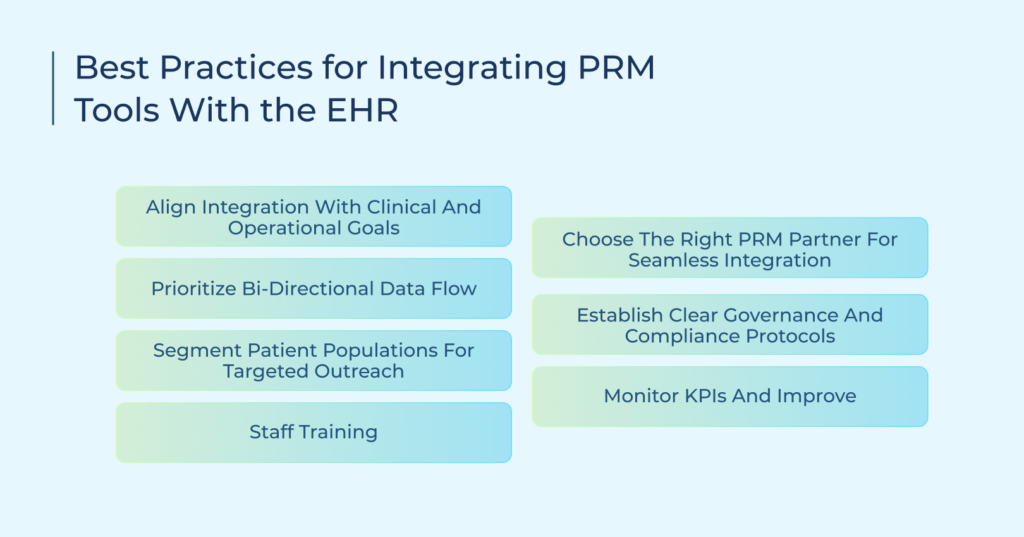
Align Integration With Clinical and Operational Goals
Healthcare organizations need to list down specific objectives that define their success. This may include a goal of reducing no-shows or readmissions, for example. Such objectives must be kept in mind when integrating PRM tools with EHR systems.
Prioritize Bi-Directional Data Flow
Focus on creating a seamless two-way communication medium between systems. If a patient reschedules an upcoming appointment through the PRM, the new information must automatically be updated in the EHR. This maintains consistency and helps reduce administrative burden, or else staff will end up spending long hours managing duplicate entries. As another example, when doctors add any notes about patients, the information must flow from the EHR to the PRM on the fly.
Segment Patient Populations for Targeted Outreach
Also considered a benefit of integrating PRMs with EHRs, creating meaningful patient groups using clinical data enables providers to deliver more personalized communication, targeted education, and timely outreach based on specific health conditions, risk factors, or care milestones. For instance, a group of diabetic patients makes it easy to send dietary tips to keep sugar levels down.
Staff Training
Provide practical training on both systems. Front desk staff need different training from clinical teams, so document common workflows and create quick reference guides. Consider creating role-specific training modules that lead to a reduction in staff questions in the early stages of the integration roll-out.
Choose the Right PRM Partner for Seamless Integration
Refrain from choosing a solution at random. Check with other healthcare organizations using your EHR system for references. Their experience just might provide valuable information about scalability, ease-of-use, support, cost, and other factors. Verify all this information before making your final selection.
Establish Clear Governance and Compliance Protocols
Every healthcare organization must have formal policies in place for sharing data between the systems. Define which staff can access what information, how patient consent flows between platforms, and how you maintain HIPAA compliance following a PRM-EHR integration.
Monitor KPIs and Improve
Keeping an eye on how your integrated systems are performing is important for long-term operational efficiency. Use metrics specific to your organization and goals to measure success. This confirms how big a chance the integration has made, and what areas and workflows can be further optimized.
Most of the top PRMs have a built-in dashboard that gives a holistic view of everything, such as showing which departments need additional support.
Understanding the Difference Between Embedded and Integrated Systems
While healthcare organizations often use “integration” as a general term for their systems, the terminology often blankets critical technical differences that affect daily operations.
Integrated Systems connect EHR and PRM platforms through external data bridges, meaning the EHR remains separate from the PRM. It requires:
- Staff toggle between separate systems.
- Data syncs periodically, creating lag time.
- Updates in one system may not appear immediately in another.
- Technical teams maintain multiple connection points.
Embedded Systems build PRM functions directly within the EHR, providing:
- Clinicians work entirely in one interface.
- Patient communication history appears alongside clinical data.
- Staff need to learn only one system.
- IT teams manage a single security framework.
Based on these differences, healthcare organizations can decide whether to switch from integrated to embedded PRM solutions. Remember that the right approach always depends on what your current workflow needs, but with embedded systems, patient communication histories become available directly in the clinical view. This is highly significant because staff can directly see missed appointment patterns alongside vitals without switching screens or platforms.
Bridging the Gap With Patient Relationship Management
EHRs are powerful, but not perfect. A modern PRM platform like TeleVox’s Smart Agent bridges the engagement and operational gaps left by traditional systems. It integrates your EHR, CRM, contact center, and RCM systems into one intelligent platform.
Powered by AI, our specialized solutions streamline critical processes such as referrals, appointment scheduling, intake, payments, readmission reduction, and reputation management, all while delivering personalized, data-driven communication.
By leveraging our AI-driven PRM solutions alongside EHRs, healthcare facilities can build stronger relationships with their patient population, leading to better health outcomes and improved financial returns for providers.
It’s not just about managing data. It’s about caring for patients every step of the way. Hence, take the next step in transforming patient engagement. Learn how TeleVox can future-proof your healthcare operations by scheduling a demo today.



