Healthcare is changing because patients are changing. They’re no longer satisfied with being numbers in…

How to Ensure an Effective Referral System as a Healthcare Provider
A referral system in healthcare is more like a bridge than paperwork. You are essentially carrying patients from one node (their primary doctor) to the next (a specialist) without losing them along the way. However, when that bridge weakens, the damage is felt on both sides. Providers lose revenue while patients lose trust as well as their health.
Recent figures show just how costly the cracks can be. In the U.S., hospitals are losing between 10 and 30 percent of revenue when referrals leak out of the network, adding up to hundreds of millions of dollars each year.
In the UK, nearly 3 million referred patients were left waiting without any specialist care as of August 2025, a stark reminder that inefficiencies translate directly into poor patient experience.
This blog will explore why an effective referral system matters and how healthcare providers can build one that is both reliable and patient-centered.
What Are Referral Systems in Healthcare?
A referral system is your pathway to get patients the specialized care they need. When a primary care doctor spots something beyond their expertise, they send the patient to a specialist who can handle that specific condition.
The best referral systems track everything from start to finish. They ensure the specialist gets your records, confirm you actually show up for the appointment, and bring the specialist’s findings back to your primary care doctor.
Modern healthcare referral systems keep updated lists of which specialists are available, what conditions they treat, and how quickly they can see patients. They also set up automatic reminders for patients and follow-up alerts for providers.
Common Types of Referrals Used by Healthcare Providers
Referrals come in many types depending on what patients need and how their organizations work.
Internal referrals happen within the same healthcare system. These move faster because everyone uses the same systems and can easily share your records.
External referrals send patients to specialists outside your healthcare organization. This requires more coordination because different systems need to share information and work together on your care plan.
Urgent referrals are for patients who need specialist care immediately, and hence, ensure they are seen as quickly as possible.
Routine referrals follow standard scheduling timelines because their cases are not emergencies.
Consultation referrals ask specialists for their opinion. They examine the patient and send recommendations back to the primary care doctor. The patient usually continues care with their regular physician.
Transfer referrals hand over complete responsibility from one provider to another. Patients with complex conditions that need ongoing specialist management get transfer referrals. The specialist becomes their main doctor for that condition.
Why Is an Effective Healthcare Referral System Important?
Poor patient referral systems create hurdles for everyone involved. They lead to missed appointments and, most importantly, cause doctors to lose track of their patients.
Keeping Revenue In-House: When referrals leak outside your network, you lose money. Patients referred outside often stay in those external networks for future care, creating permanent revenue loss. So, it’s best to keep these patients within your organization.
Patient Safety Comes First: Your main goal is to get patients the specialist care they require as soon as possible. But, if your referring data fails to reach specialists, your patients can get worse without the proper treatment.
Meeting Requirements and Standards: Care coordination and referral processes should be documented by healthcare organizations for regulatory purposes. Quality reporting standards and proper record maintenance are required by effective referral systems in healthcare.
Standing Out: Healthcare markets with multiple provider options make referral management a way to stand out. Organizations with smooth referral processes attract more primary care physicians and keep patients within their networks.
Provider networks that show effective care coordination appeal to insurance companies and employer health plans. These relationships generate steady patient volume and more referral opportunities.
Key Components of an Effective Referral System
Your referral system in healthcare needs three core pieces to work properly. Get these right, and patients move smoothly between primary care and specialists.
Key Referral Criteria
You need clear rules about when to refer patients. Without them, you’ll either send everyone to specialists or miss patients who really need specialty care.
Set specific triggers for different conditions. Chest pain with certain symptoms means cardiology within 24 hours. Diabetes with complications above specific thresholds goes to endocrinology.
Create urgency levels that match reality. Emergency referrals need same-day specialist contact, while routine referrals can wait weeks. Don’t promise 48-hour referrals if your specialists book three weeks out.
Tracking and Monitoring
Track every referral from creation to completion. Too many patients get lost between the referral and the actual specialist visit.
Make sure to confirm the specialist received your referral and that the patient scheduled a visit. Also, follow up when patients don’t show up.
Use automated alerts for overdue referrals. Your patient referral system should flag missing specialist reports or appointments that never happened. These alerts help staff catch problems before they get worse.
Generate monthly reports on completion rates and wait times. This data shows you where your system breaks down and needs fixing.
Coordination and Communication
Include relevant history, current medications, recent test results, and your specific questions with every referral.
Note that your hospital referral system works best when everyone communicates clearly and quickly throughout the patient’s care journey.
For that purpose, specialists must report back after seeing your patients. They should answer your questions and provide clear recommendations. They need to specify whether they’re taking over care or sending the patient back to you.
How to Build an Effective Referral System for Your Healthcare Organization
Setting up a referral system in healthcare doesn’t have to be overwhelming. You just have to break it down into manageable steps.
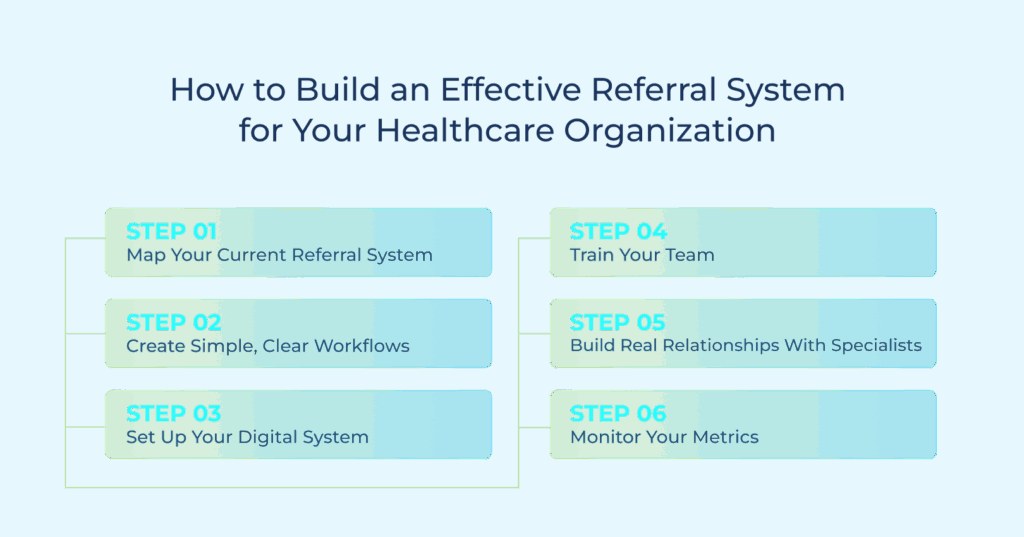
Step 1: Map Your Current Referral System
Walk through your current referral process from start to finish. You’ll probably discover it’s messier than you thought.
Track a few referrals from creation to completion, and see at what points data gets stuck or where delays happen.
You can ask your front desk staff and doctors where they spend the most time chasing down information. Your patients can also tell you plenty about scheduling issues and missed appointments.
Step 2: Create Simple, Clear Workflows
Create simple workflows for different referral types instead of a single, bloated template. Your intake forms should capture essential information every time.
Focus on what the specialist needs to know, not just what’s easy to collect. And remember: every extra hand in the chain is another point where messages can get lost, so keep your referral path lean and direct.
Step 3: Set Up Your Digital System
Choose systems that connect primary care and specialist offices. Shared medical records eliminate the need to recreate patient information multiple times.
It’s also good to implement automated referral tracking that flags overdue referrals and missing reports. Your patient referral system should alert staff when specialists don’t receive referrals or patients miss appointments.
Make sure your new software integrates with your existing systems. Staff shouldn’t need to log into five different systems to process one referral.
Step 4: Train Your Team
Walk your whole team through the new process. Your receptionist needs to know how specialist scheduling works, and your nurses need to understand what information specialists are looking for.
It’s good practice to run trial runs before going live. This allows you to spot problems during training, not when real patients are waiting. This is also where your staff can make cheat sheets for the tricky procedures.
Step 5: Build Real Relationships With Specialists
Sit down with the specialists that you refer to on a regular basis. Discuss what they want out of referrals and how soon they are able to get back to various types of cases. These conversations help you catch problems before they turn into major issues.
Step 6: Monitor Your Metrics
Watch the numbers that matter. How many referrals actually result in appointments? How long do patients wait for specialists? Are patients happy with the process?
Look at your reports every month. If one specialist always has long wait times or high no-show rates, you need to address it. Don’t wait until patients start complaining.
Your hospital referral system needs regular attention. What works today might not work next year as your patient volume changes or specialists retire.
Best Practices for Implementing the Right Referral System in Healthcare
You require a structured process that closes communication loops, minimizes delays, and keeps patients satisfied during the referral process.
Define Clear Referral Protocols and Guidelines
Your staff needs to know the details of every referral order. Create a simple checklist that covers patient history, why you’re referring them, what tests you’ve already done, and what specific question you want the specialist to answer.
Don’t leave room for guesswork. Assign specific people to handle different types of referrals. When everyone knows their role, nothing gets missed.
Also, set meaningful deadlines. Emergency referrals should always go out the same day. Routine cases can be processed within two business days. Write this down and stick to it.
Leverage Technology for Efficient Referrals
Your EHR system should connect directly to your referral platform. This means patient information flows automatically instead of someone retyping everything. So, when the specialist responds, both systems update at once.
Get referral tracking software that works on phones and tablets. Confirm that they create an automatic paper trailer to help you during audits.
Digital platforms provide real-time updates, meaning your staff can check on referrals while performing their other tasks, allowing you to catch problems before patients start complaining.
Establish Effective Communication Channels
Set up automatic reminders when specialists haven’t responded within your timeframe, and create a direct phone line between your office and frequently used specialists. Skip the front desk runaround when you need quick answers about patient care.
Ensure HIPAA Compliance and Data Security
Your hospital referral system needs bulletproof HIPAA security for patient information. Every message, file transfer, and system login should be encrypted, with no exceptions.
Choose software vendors who understand healthcare regulations. They should provide automatic backups, user access controls, and detailed logs of who accessed what information when.
Train your team on HIPAA-led secure communication. Personal email accounts are off-limits for patient information. Teach them to recognize phishing attempts and suspicious requests for patient data.
Evaluate and Optimize the Referral Process Regularly
Track the right metrics to confirm your referral process is working as intended. Monitoring referral completion rates, provider response rates, etc., helps you understand how smoothly patients are being handed off. It also helps spot service gaps and bottlenecks.
Make sure to collect patient feedback about their experience. They are an excellent source of identifying pain points that you might miss, such as confusing instructions and long wait times.
Common Challenges and How to Address Them
Your referral system in healthcare will hit roadblocks. It’s not a matter of if, but when. Here’s what goes wrong most often and what you can do about it.
Administrative Overload
Your staff drowns in referral paperwork. Forms keep piling up on the desk and patient information gets entered multiple times across different systems. It’s easy for someone to forget to include something important.
Solution: Connect your referral software to your EHR system. Your patient data will transfer automatically, allowing your team to focus on patients instead of the paperwork around the office.
Communication Breakdowns
Consider this scenario. You send a referral to a cardiologist, but they call back asking for information you’ve already included. The added confusion reaches the patient as well who shows up two weeks later with new medications. This happens more often than you think.
Solution: Build a standard referral template that includes everything specialists need. Set up automatic alerts that remind specialists to send feedback reports. It’s also important to create a direct communication line for urgent questions.
Insurance Authorization Nightmares
Your patient referral system can come to a halt waiting for insurance approvals. It’s common for your authorization request to sit in some insurance company queue for weeks. Meanwhile, the patient’s condition gets worse, and your staff wastes hours calling for status updates.
Solution: Submit your authorization requests digitally with complete medical records attached. The best insurance companies have online portals that track approval statuses. It’s also good to have backup specialists ready for patients with different insurance plans.
Incompatible Technology
Your office uses Epic, the specialist uses Cerner, while the hospital uses something completely different. Hence, your patient information exists in three separate systems that can’t share data. Everyone asks the patient the same questions over and over.
Solution: Choose referral management platforms that work with multiple EHR systems. Look for software that can pull data from one system and push it to another automatically. Your hospital referral system needs to connect all the pieces.
How TeleVox Helps You Create Efficient Referral Systems
Every referral is a moment of trust where patients expect to move from one provider to the next without confusion or delay. TeleVox makes that handoff seamless with secure, automated referral management built to meet HIPAA standards. We keep every referral organized, complete, and on track.
With the right information reaching the right specialist at the right time, patients stay confident and satisfied while providers avoid costly leakage. At the same time, our automation and EHR integration reduce manual handoffs, simplify coordination, and lift the administrative burden from staff.
And while the platform handles the process itself, our SMART Agent plays a supporting role by answering patient questions, delivering intake forms, and reducing back-and-forth with staff.
Remember that the simplest step you can take to fix the cracks in your referral process is the most effective one. Schedule a demo and see how TeleVox streamlines referrals from start to finish.



