A patient engagement platform is a digital hub that makes it easier for patients to…

HIPAA Violation Examples and How to Avoid Them as a Healthcare Provider
Imagine throwing away an old hard drive that exposed hundreds of patient records or sending a single email to the wrong person that turned into a six-figure penalty. These aren’t rare accidents. They’re common examples of what happens when organizations overlook healthcare regulations.
The Health Insurance Portability and Accountability Act (HIPAA) exists to protect patient privacy and keep sensitive health data secure. For healthcare providers, these legal requirements spell a responsibility that defines patient trust.
Today, we’ll look at real-world HIPAA violations that have cost organizations money, credibility, and peace of mind, and more importantly, what you can do to make sure your practice doesn’t end up on that list.
Understanding the Impact of a HIPAA Violation
Breaking any rules set by HIPAA goes way beyond paying a small fine. Your health organization can end up paying millions, depending on the violation.
In 2024 alone, the Office for Civil Rights closed 22 cases with financial penalties of more than $9.9 million. That is just the beginning.
You damage your professional reputation and expose yourself to potential patient lawsuits. You might also have to endure years of government oversight before being allowed to operate freely.
In some cases, you can even lose your license altogether. Hence, understanding why compliance matters here starts with understanding all of these consequences.
- The most serious cases can slap fines that reach over $2 million annually.
- Criminal charges can be imposed with up to 10 years in jail if found guilty of knowingly exploiting patient data for financial reasons.
- Patient class-action lawsuits translate to more fines and litigation that could take years.
- Insurance premiums rise following HIPAA breaches, with the majority of insurers declining to become partners until your lawsuits are settled.
- Patients lose confidence in you and begin seeking other providers, so you lose money.
- The indirect costs creep up fast when you include attorney fees, IT security upgrades, public relations initiatives, and worker training programs.
HIPAA Violation Examples Every Healthcare Provider Should Know
Even the most minor violations can have HIPAA breathing down your neck, costing your organization millions in fines. Your staff may also have no clue that they’re breaking the rules, making it critical that all providers understand how to follow healthcare regulations.
Unauthorized Access to Patient Records
Just because you have access to a file doesn’t mean you should. Many employees sometimes get curious about the medical records of a friend, family member, celebrity patient, or even themselves.
But if you’re not directly involved in that person’s care, you’re not allowed to look. It’s one of the most frequent HIPAA violation examples in healthcare.
How to Avoid This Violation
Start with audit logging to track who opens which files and when. Have role-based access set up alongside so that your employees only access records they’re meant to see.
Lost or Stolen Devices Without Encryption
You might think that you’re not at fault if someone steals one of your staff’s laptops, but you are. If that laptop has patient records on it, thieves can sell it on the black market. This applies to all storage devices like phones, tablets, portable drives, etc.
A highly relevant real-world case example would be Feinstein Research paying $3.9 million after someone stole an unencrypted laptop from an employee’s car.
How to Avoid This Violation
Turn on encryption for every device that stores patient data. It makes the data useless even if thieves manage to get their hands on it. Strong passwords or fingerprint access add another line of defense, along with remote wiping capabilities.
However, it’s better to never save any patient file on a personal device. Use secure remote access if your staff needs to work from home.
Social Media HIPAA Violation Examples
Healthcare professionals can share patients’ details online without regard to their privacy. Even a harmless picture can be a serious offense. Basically, anything that can identify patients, like names, rare conditions, specific treatment dates, job hints, or locations, is a big mistake.
Manasa Health Center paid $30,000 after responding to negative online reviews by disclosing patient mental health information. They thought they were defending their services, but broke the law instead.
How to Avoid This Violation
You need to place a strict ban on all social media posts about patients or your organization in general. Make it crystal clear to your staff that even vague references can violate HIPAA. That hallway selfie of yours? It might show a patient’s name or chart in the background. There’s no room for error here.
Improper Disposal of Records
You can’t just throw patient files in a regular trash bin. The same goes for hard drives or any other storage device. This is because your patients’ data can still be recovered through various software even if you have deleted them.
ShopRite ran into trouble when they threw away old electronic devices from their pharmacy counters. Those devices still had customer signatures and purchase records on them.
How to Avoid This Violation
Use shredders to destroy patient records or files. This should take place on-site under secure observation. No one should be allowed to take papers home to shred there.
For electronic devices, physically destroy storage devices and use proper software to completely wipe all data beforehand.
Most healthcare organizations partner with vendors to securely destroy patient records. They provide certificates after the job is done to help you comply with auditors.
Delayed or Denied Access to Patient Records
Patients have the legal right to their medical records. If someone sends a request for a deceased loved one’s records, you’re bound by law to comply within 30 days. Delaying or downright refusing them is a severe HIPAA violation. This often happens because nobody’s tracking requests, or the process is too complicated.
How to Avoid This Violation
Have a separate team to handle all record requests. Digital record keeping makes this easier since you don’t have to dig through file rooms. Train your team to follow a simple process: receive a request, verify the identity, pull the records, and send them.
Failure to Log off Shared Systems
Yet another common HIPAA violation example is authorized staff forgetting to log off their systems. Consider a doctor accessing patient files on his laptop, but has to suddenly dash to the exam room. Someone else walking by might see whatever’s on their screen. This leads to two big issues: anyone can access those records without permission, and it becomes unclear who actually did what in the system.
How to Avoid This Violation
Configure your computers to automatically log out after 5 or 10 minutes of inactivity. This can be done on a large scale via the main network administration. You don’t have to physically set each computer in the building. You can also place small signs near shared computers to remind everyone to log off.
Mishandling of Data by Business Associates
Your third-party vendors can cause HIPAA violations even when your own staff does everything right. These business associates include billing companies, IT support, cloud storage providers, medical transcription services, and answering services. If they mishandle patient data, you’re both in trouble.
Gulf Coast Pain Consultants paid over $1 million after a fired contractor kept accessing their systems with old login credentials. The contractor stole information for tens of thousands of patients and filed thousands of fraudulent Medicare claims.
How to Avoid This Violation
Keep a check on your vendors after you hire them. You should always research them before signing a contract, but even the best can make mistakes. Ask them about their security measures, certification proofs, and how they do internal audits. Importantly, revoke all access when you both part ways. Don’t wait until the next week or month.
Lack of Compliant Agreements With Business Associates
This is a rather simple HIPAA violation, but still a serious one at that. You must have a signed Business Associate Agreement (BAA) before any vendor handles patient information.
A handshake deal or verbal agreement doesn’t cut it. BAAs spell out exactly what information the vendor can access, how they must protect it, and what happens if they cause a breach. Without this paperwork, you’re both violating HIPAA from day one.
How to Avoid This Violation
Never let a vendor touch patient data until you have a signed BAA. Some vendors will push back or claim they don’t need one. If they refuse to sign, find a different vendor. It’s that simple.
Missing or Incomplete Risk Analysis of the Organization
A risk analysis is basically a security audit where you examine all the ways patient data could be exposed or stolen. You look at your computer systems, your building security, your employee practices, everything. Then you document what you found and make a plan to fix the problems.
Not doing this analysis is itself a HIPAA violation. The government wants to see that you actually thought about security and took it seriously.
How to Avoid This Violation
Plan a full risk assessment once a year and get your IT, compliance, and security teams involved. Check that every device and system handling patient data is secure.
And remember, it’s not something you check off once and move on from. Update your assessment every time you bring in new tools, update systems, or change how your team works. Staying proactive saves you from big breaches and even bigger fines.
How to Handle a HIPAA Breach the Right Way
Data breaches shouldn’t happen, but if they do, you have 60 days to address the problem or else face penalties on top of the damage the breach already caused.
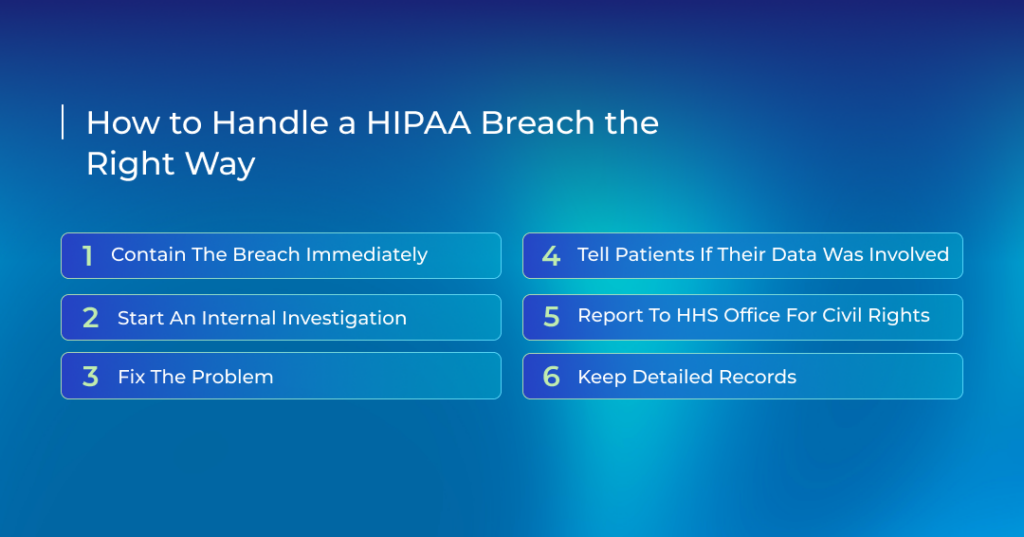
- Contain the breach immediately
- Isolate the breached system.
- Change access credentials for compromised accounts.
- Preserve evidence for investigation.
- Start an internal investigation
- Confirm who saw what, how, and if the risk has been mitigated.
- Interview your staff and review the audit logs.
- Fix the problem
- Take the necessary corrective actions.
- Update your policies if they failed you.
- Provide additional staff training so that the same mistake doesn’t happen again.
- Tell patients if their data was involved
- Send letters within 60 days explaining the breach, what information got out, and what you’re doing about it.
- If you can’t reach 10 or more patients by mail, post a notice on your website for 90 days.
- Report to HHS Office for Civil Rights
- Big breaches (500+ people): report immediately through the OCR portal.
- Smaller breaches (under 500): you can wait and report by March 1 of the next year.
- Keep detailed records
- Write down when you discovered the breach, how you controlled it, and what the investigation found.
- Keep copies of all notifications you sent out.
- Prepare a final report with your remedial actions.
Real-World Examples of HIPAA Violations and Consequences
Here are three examples of HIPAA violations, each including what happened, who was involved, the consequence, and what could have prevented it:
Montefiore Medical Center, one of New York’s largest non-profit hospital chains.
A hospital staff member stole and sold the records of 12,517 patients. The hospital neither had any risk analysis nor ePHI system-monitoring procedures.
MMC had to pay $4.75 million in settlement fees in 2024.
What could have prevented it:
- Conducting and acting on a full risk analysis of ePHI systems.
- Having system-activity monitoring systems.
- Giving users the least amount of access to patient data.
PIH Health, Inc., a health-care network in California.
The network’s employees were caught in a phishing attack by clicking on email links they shouldn’t have and it exposed the health information of 189,763 patients.
A settlement of $600,000 and a two-year corrective action plan were the result.
What could have prevented it:
- Performing a complete and accurate risk analysis of ePHI systems.
- Having timely breach-notification procedures.
- Educating the staff on phishing dangers and protecting email access.
Holy Redeemer Family Medicine, a family-led practice in Pennsylvania.
A patient permitted the practice to send a specific test result to their employer. However, Holy Redeemer sent the patient’s full medical record.
The consequence was a settlement of $35,581 in 2024, plus a corrective action plan.
What could have prevented it:
- Ensuring disclosures align strictly with what the patient authorizes.
- Establishing clear internal policies and checklists for authorizing external disclosures of PHI.

How Does Televox Ensure HIPAA Compliance for Its Platform?
Televox centralizes all patient communications into a secure hub that meets regulatory standards. Every text, chat, or call flows through controlled access points, so only authorised staff see sensitive data.
On top of that, our platform encrypts data during both transmission and storage, protecting PHI from interception or unauthorized access.
To give you a clear view of how it works:
- Every user gets role-based access, so only the right people can view or handle patient information.
- HIPAA-compliant messaging secures every interaction. Every action (who sent what, when, and how) is logged automatically, giving your compliance team a clear audit trail for reviews or inspections.
- The HiTrust-certified architecture integrates with your EHR, keeping your existing workflows intact while protecting PHI at every stage.
- You can also manage patient intake, check-ins, and insurance verification through secure links and dashboards, creating a safer hospital communication process from start to finish.
Schedule a demo if your healthcare organization wants tools that handle communications while being compliant.



