Televox is proud to announce that its Enterprise Edition SMS solution has been awarded Gold…

Benefits of Interprofessional Collaboration in Healthcare
When healthcare teams don’t communicate well, patients feel it. Delays happen. Details slip through. Decisions take longer than they should. The fact is that poor collaboration between providers often leads to longer stays, repeat visits, and missed follow-ups.
Most of these issues come down to gaps in coordination. One team doesn’t know what the other is doing. The patient ends up repeating the same information or waiting for updates that never arrive.
Every provider should take this seriously. When staff share information clearly and respond quickly, care improves. This article looks at what works and why better teamwork makes a difference.
How Interprofessional Collaboration Works in Healthcare
Healthcare providers are not a one-person affair. They involve several diverse teams that play important roles in bringing unique specialities to the table.
When doctors begin morning rounds, nurses brief them on the status of the patients. Physicians from various branches can exchange notes and histories using the same EHRs.Medical leaders attend conferences to discuss complex cases and bring new perspectives to light.
These are just some examples of interprofessional collaboration in healthcare, each one sharing information and expertise with the shared goal of improving care delivery and outcomes.
Why Is Team Collaboration Important?
For healthcare organizations, strong teamwork improves workflow. Staff spend less time searching for information or fixing miscommunications. This saves time and reduces frustration for both workers and patients.
Collaborative teams also make more balanced decisions. A single provider might miss important considerations that another professional would notice. Multiple perspectives lead to more complete care plans. Hence, when teams work together effectively, they catch mistakes before they reach patients.
This collaborative approach, though, relies on crystal clear communication channels and coordination. When done right, patients report higher satisfaction ratings as they receive consistent information and feel their needs are better addressed.
Key Benefits of Interprofessional Collaboration in Healthcare Organizations
Collaboration connects professionals from different specialties, improves care coordination, and supports staff wellbeing. This team-based approach aligns perfectly with a modern healthcare organization’s focus on patient outcomes. It actually forms your core value-based models.
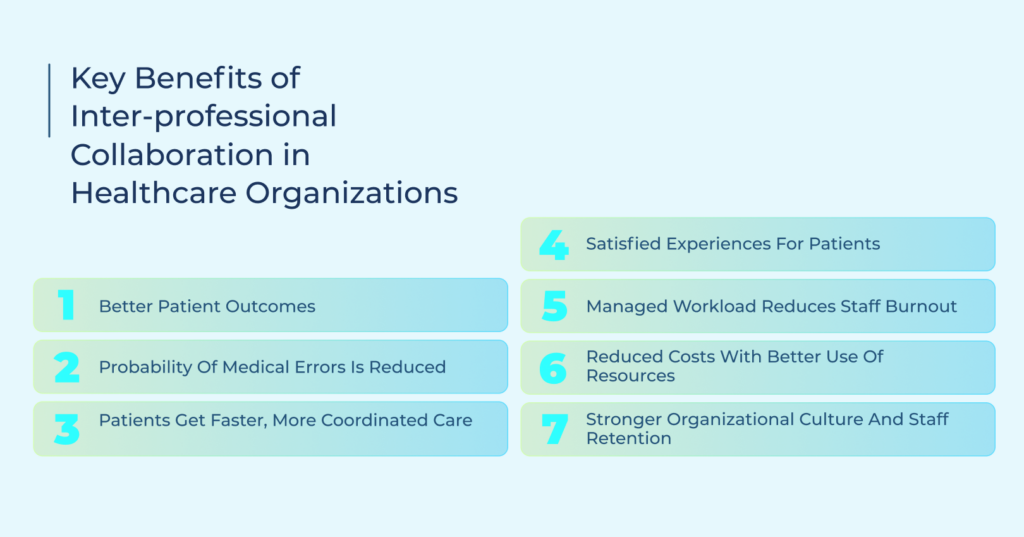
1. Better Patient Outcomes
A board of multidisciplinary professionals will always demonstrate greater treatment accuracy compared to decisions made by a single physician. We can take several use cases as examples to further highlight the importance of a collaborative healthcare environment.
Physicians and specialists contribute different diagnostic perspectives, catching issues that might be missed by a single provider. Nutritionists design meal plans that support medical treatment goals, working in tandem with healthcare providers toward patient well-being.
Pharmacists identify potential medication interactions before they cause complications. Physical therapists add mobility assessments that help patients recover function faster.
2. Probability of Medical Errors is Reduced
As already noted above, team communication creates multiple checkpoints that catch potential mistakes and errors before they reach patients. Structured handoff protocols ensure critical information transfers between shifts, and standardized communication formats like Situation-Background-Assessment-Recommendation (SBAR) prevent misunderstandings between departments. It’s also common practice to do regular team huddles to bring attention to changing patient conditions.
3. Patients Get Faster, More Coordinated Care
The importance of collaboration in healthcare is evident in the reduced average length of stay following the implementation of structured team-based processes. This is because clear communication channels speed up test result views and treatment decisions, preventing duplicate procedures. Discharge planning starts earlier since all necessary providers have already shared their input. Collaboration saves a lot of time and resources across settings.
4. Satisfied Experiences for Patients
Patients notice when care teams work well together. Having their questions answered promptly by the appropriate team member and seeing them spend more time on care and less time on asking the same questions makes patients comfortable, leading to positive patient experiences.
5. Managed Workload Reduces Staff Burnout
Interprofessional collaboration is also beneficial for the healthcare staff. Since everyone shares responsibilities, the burden of delivering quality care gets divided more evenly. Tasks match the appropriate skill level of each team member, and professionals support each other during high-stress situations.
Team members also cover for each other during breaks, time off, or emergencies. This unified approach reduces burnout and helps staff process emotional strain during difficult cases.
6. Reduced Costs With Better Use of Resources
Collaboration creates financial efficiencies. For instance, shorter hospital stays and fewer readmissions due to coordinated discharge planning mean fewer resources spent. It’s not just about reducing cost. Healthcare providers get to better manage their resources and specialties.
7. Stronger Organizational Culture and Staff Retention
Teams that work well together create positive workplace environments, which helps providers report higher retention rates. New employees receive better mentorship and integration, and staff develop meaningful professional relationships across departments. The boosted morale significantly improves operational efficiency across departments.
Barriers to Effective Interprofessional Collaboration in Healthcare
Technical limitations, cultural factors, and organizational structures can create roadblocks for effective team-based approaches. These barriers affect patient care quality and staff satisfaction, but can be addressed through targeted strategies.
Communication Silos Across Departments
Most healthcare providers have separate communication systems for different departments. This ends up causing delays and conflicts as one department might have different documentation standards while another is limited to paper-based communication. Worse, providers using incompatible EHR systems are unable to share data, creating bottlenecks and data silos.
How to Address This Barrier:
It’s always good practice to implement unified communication platforms with standardized formats. Create shared access points for patient information with appropriate security. HIPAA compliance is mandatory here. You can also establish regular cross-department meetings for critical information sharing.
Hierarchical Structures and Role Confusion
Traditional healthcare hierarchies often block effective teamwork. This is because physicians are accustomed to making unilateral decisions without input from other professionals, nurses hesitate to speak due to authority tiers, and overlapping responsibilities without clear delineation of tasks.
How to Address This Barrier:
Healthcare organizations can start by creating clear role definitions for each team member with accountability maps. Implement communication structures where all team members can voice concerns regardless of their place in the authority hierarchy.
Insufficient Training in Team-Based Care
Education often fails to prepare healthcare professionals for teamwork. Medical and nursing schools traditionally emphasize individual competence over team skills. Most students face limited opportunities to practice interdisciplinary communication, and there are few formal training sessions on conflict resolution or collaborative decision-making.
How to Address This Barrier:
The best course of action here is to provide continuing education on team communication techniques. Create simulation scenarios to practice problem-solving and make the staff comfortable in real-life situations. It’s also important to establish mentorship programs pairing professionals across disciplines.
Resistance to Change and Organizational Inertia
Established organizations often resist improvements to collaborative structures. They are comfortable with familiar workflows despite their limitations. There’s also the fear of learning new workflows and increased workloads. A lack of visible leadership to support collaboration initiatives can also act as an obstacle.
How to Address This Barrier:
Start with small pilot projects demonstrating clear benefits, and share concrete success metrics and patient outcomes. Head on to identify and support the best staffers in each department. That said, remember to provide adequate time and resources for teams to adapt to the new change.
Role of Technology in Improving Cross-Team Collaboration
An efficient interprofessional collaboration environment wouldn’t be possible today without the right technology. Modern communication systems share up-to-date patient records with relevant team members, secure messaging for real-time consultations between providers, support virtual meetings and telehealth appointments, and power mobile healthcare apps for care on the go. These tools streamline coordination, reduce delays and errors, and ultimately improve patient outcomes.
How TeleVox Helps Your Teams Work as One
True collaboration in healthcare doesn’t happen by chance. It requires clear, smart, and seamless communication across every role. That’s exactly what TeleVox delivers.
With SMART Agent, our conversational AI-powered virtual concierge, your teams gain a centralized digital front door that keeps everyone connected and every patient supported 24/7.
From scheduling appointments and answering FAQs to routing inquiries to the right professional, SMART Agent automates routine tasks so your people can focus on what matters most: delivering the best care possible without bogging down your staff.
When every professional has the time, clarity, and tools to do their best work, your entire system thrives.
Ready to automate your interprofessional collaboration? Schedule a demo today and see why TeleVox leads the way in smarter healthcare teamwork.



